Boost Revenue With RPM Logix's RPM & CCM AI Tools
RPM Logix utilizes an artificial intelligence (AI) algorithm that tracks patient billing progress throughout the month. We factor in allowable minutes based on the patient’s insurance, and which programs they’re enrolled in.
Scenario 1
We’re approaching month-end. An RPM patient has 61 minutes documented, and has an insurance cap of 80 minutes. The patient is due for a 10-minute education follow-up call. If that 10-minute call is placed on the last day of the month, it will not be billable because no minutes count until the next billable threshold (80 minutes is met). The RPM algorithm will schedule that next elective phone call for a day later at the beginning of the new month, when it will be fully billable.
THIS IS ONLY DONE FOR ELECTIVE PHONE CALLS. ANY PATIENT CALLS OR READING ALERTS WILL ALWAYS BE RESPONDED TO IMMEDIATELY.
Scenario 2
A Medicare patient is dual-enrolled in RPM and CCM programs (specifically permitted in the CMS rule: as long as minutes for each program are clearly separated, RPM Logix software assures compliance). The patient has an 80 minute cap on their insurance allowable for RPM, and 60 minutes for CCM, and is seeing our diabetes educator for diabetes prevention. A total of 100 minutes for the month is documented. RPM Logix will record the first 80 minutes under RPM, and document the spill-over 20 minutes into CCM. Education is optimized, and reimbursement is optimized as well – all while staying 100% compliant.
Scenario 3
Avoid the February billing trap. CMS rules specify that RPM time-based codes 99457 and 99458 can only be billed once per calendar month. This means the date of service can be any day of the month.
CPT code 99454 for monthly device readings has a DIFFERENT RULE. It can only be billed after a 30-day interval has elapsed from the prior month’s date of service for this code. Let’s say your January date of service is January 31. Come February, if you submit the 99454 claim with date of service Feb 28, it will be rejected!
RPM Logix’s algorithm will push the next date of service to March 2, so you’ll be in compliance with this 30-day interval requirement. Subsequent months’ dates of service will also be adjusted so you won’t have claims rejected for procedural errors.
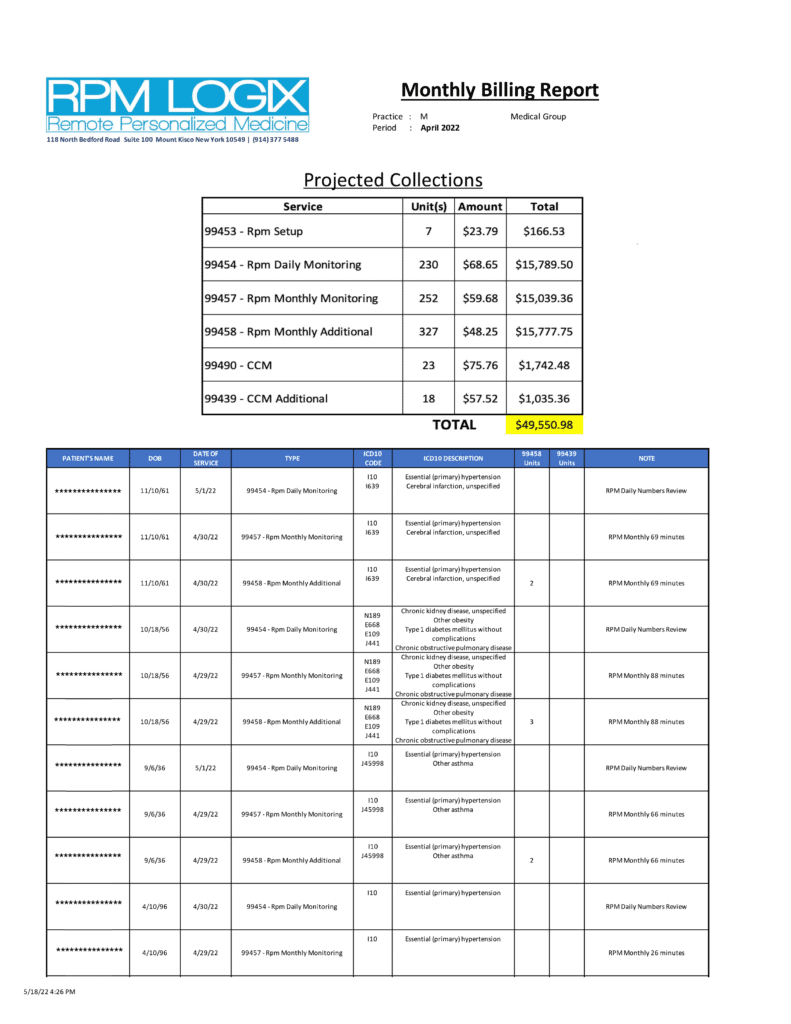
After each month-end, RPM Logix will provide you with a COMPREHENSIVE Billing Report to capture all billable activity, and assure compliance. Everything that’s required for accurate billing is on the report- Name, DOB, ICD-10 Diagnosis Codes, CPT Codes with accurate units noted for add-on codes. The all important date of service is listed as well. This is critical. While RPM and CCM share monthly billing cycles, certain codes with their add-ons must show the same date of service or they’ll be rejected.
We will also provide you with a projected collection total based on your local Medicare fee schedule.
Below is a page from a live report for a practice billing approximately 250 RPM patients.
RPM Logix is licensed to access the Medicare HET-S database
HIPAA Eligibility Transaction System (HETS)
The HIPAA Eligibility Transaction System (HETS) allows us to check Medicare beneficiary eligibility data in real-time on your behalf. This allows for up-to-date eligibility screening, and saves time and money avoiding services for ineligible patients.
Leverage data-mining techniques to extract all RPM-eligible and CCM-eligible patients, and populate them inside your CCM portal.

